ARTICLE AD BOX
Health officials in the United States are sounding the alarm over the rise of so-called “nightmare bacteria” – dangerous germs resistant to nearly all available antibiotics. The Centers for Disease Control and Prevention (CDC) has reported a concerning surge in these infections, which are harder to treat, spread quickly in healthcare settings, and can even turn deadly.But what exactly is this “nightmare bacteria”? How can you recognize its early warning signs, and most importantly, what can you do to protect yourself and your family?
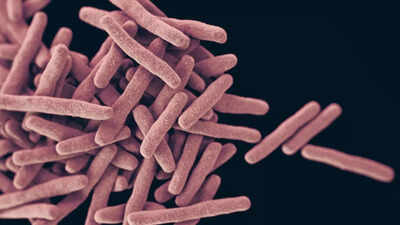
What is “nightmare bacteria”?
The term “nightmare bacteria” is used to describe Carbapenem-resistant Enterobacteriaceae (CRE). This group of bacteria, which includes Klebsiella pneumoniae and Escherichia coli (E. coli), has developed resistance to carbapenems – a class of “last-resort” antibiotics usually reserved for severe infections.Why the name?The CDC calls them “nightmare” because they:Spread resistance genes easily to other bacteria.Cause deadly infections in the bloodstream, lungs, or urinary tract.Do not respond to most antibiotics, making treatment difficult.A key driver of the recent increase is bacteria carrying the NDM gene (New Delhi metallo-β-lactamase). This gene lets bacteria neutralize many antibiotic drugs, making them ineffective.
Some of these bacteria used to be mostly seen in patients who had medical treatment overseas, but now US cases have surged. Numbers have increased by more than fivefold in recent years for some strains.
The rise and the reasons
According to recent CDC surveillance reports, CRE causes thousands of infections each year in the US and leads to hundreds of deaths, particularly among hospitalized patients and those with weakened immune systems.
However, between 2019 and 2023, infections from these hard-to-treat bacteria rose by almost 70%, driven largely by those carrying the NDM gene. In 2023, in 29 states, there were over 4,300 carbapenem-resistant bacterial infection cases; about 1,831 of them were the NDM variety.
Very few medicines still work, and they often must be given in a hospital, via IV.But why are cases rising now?The increase in CRE infections in 2025 is tied to several factors:Antibiotic overuse: frequent or unnecessary use of antibiotics in humans and livestock has fueled resistance.Hospital spread: patients on ventilators, catheters, or IV drips are especially vulnerable.Global travel: resistant strains can move quickly across borders.Post-pandemic vulnerabilities: COVID-19 left many patients with long hospital stays and heavy antibiotic use, creating more chances for resistant germs to thrive.
Early signs of infection
CRE infections can mimic common bacterial illnesses, which makes them tricky to spot early. Warning signs depend on the infection site:Urinary tract infections (UTIs): burning sensation, frequent urge to urinate, fever, or cloudy urine.Bloodstream infections (sepsis): high fever, chills, confusion, rapid heartbeat, or very low blood pressure.Pneumonia (lung infection): cough, shortness of breath, chest pain, or fever.Because these symptoms overlap with other illnesses, lab testing is crucial to confirm if CRE is the cause. Delayed diagnosis can make treatment harder.
Why “nightmare bacteria” are dangerous
High mortality rate: Some studies show that up to 50% of bloodstream infections caused by CRE can be fatal.Limited treatment options: Only a few antibiotics, often older or more toxic ones, may work.Silent spreaders: People can carry the bacteria in their gut without symptoms, unknowingly transmitting them to others.
How to stay safe: Prevention tips
Doctors emphasize that prevention is the strongest defense against CRE infections. Here are expert-backed ways to protect yourself:Practice good hand hygiene: Wash hands thoroughly with soap and water, especially after hospital visits, using public restrooms, or caring for sick relatives.Use antibiotics responsibly: Take them only when prescribed, finish the full course, and never demand antibiotics for viral infections like colds or flu.Ask about hospital safety: If you or a loved one is hospitalized, don’t hesitate to ask staff about infection-control measures such as glove and gown use.Keep wounds clean: Even small cuts should be washed and covered properly to prevent bacterial entry.Stay informed during travel: In regions with high antibiotic resistance, be extra vigilant about hygiene and food safety.
Confidence in Covid-19 vaccine important for US: Mike Pence


.png)
.png)
.png)











 2 hours ago
3
2 hours ago
3









 English (US) ·
English (US) ·